The Future is here: Telepsychiatry as a Tool to Reach the Unreachable
Ujjwal Ramtekkar, MD, MPE, MBA, DFAACAP
Child and Adolescent Psychiatrist
Associate Medical Director, Partners for Kids
Nationwide Children’s Hospital, Ohio, USA
Global burden of child and adolescent mental health disorders is rising at an alarming rate. There has also been rapid growth in pharmacological and behavioral treatment modalities to address common psychiatric disorders. However, the critical shortage of a trained mental health workforce including child and adolescent psychiatrists and the concentration of providers only in the larger metropolitan areas poses a significant challenge in accessing these services for many children and their families. As a result, majority of children are not receiving treatments that are deemed effective in a timely fashion. This gap in the demand, supply and access needs to be addressed with newer methods of delivering care.
Telepsychiatry has emerged as an effective way of leveraging technology to reach patients where they are. One of the most common forms is to use the two way, interactive, video conferencing to connect the provider and patient at a distant location such as homes, schools, residential centers or local clinics. The convenience of getting services virtually has reduced the barriers of travel, distance and in some cases cost. In the past decade, telepsychiatry has been adopted widely due to the reduction in technology cost, ubiquitous availability of internet and overall comfort with video-based communication through social media. However, it is not just about ‘convenience’ but also proved to deliver ‘quality.’ Several research studies have demonstrated that telepsychiatry is feasible, well accepted by providers and patients, and leads to comparable clinical outcomes in a variety of settings. Telepsychiatry has been a boon in serving families in rural areas, difficult geographic terrains and places with limited psychiatric providers.
In addition to providing direct patient care, there are several other ways in which telepsychiatry has improved access to specialty care. These include specialty consultation, live video-conferencing education for providers in local communities by experts at national and international academic centers and group consultation in the ‘hub and spoke’ model. These models not only increase access to specialty care for children, but also build capacity for the local workforce in evidence-based modalities. One such model ‘Project ECHO’ has been expanded to over 37 counties using the ‘hub and spoke’ videoconference- based learning collaborative between interdisciplinary specialist hubs and local providers in primary care or specialist ‘spokes’. There have been successful programs in child behavioral health and Autism across USA, India, Europe and Africa.
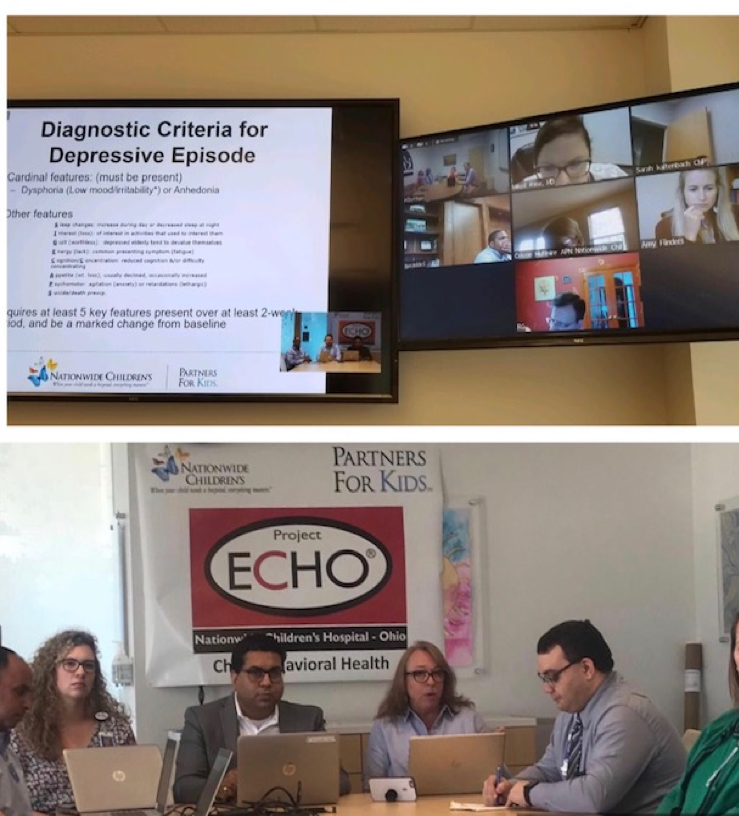
Pic 1. ‘Project ECHO Child Behavioral Health’ at Nationwide Children’s Hospital, OH, USA
Integrating verbal and non-verbal communication skills are most important in establishing a trusting relationship and a therapeutic experience over videoconferencing. Therefore, it is crucial to develop cultural awareness, understanding social factors and nuances in communication preferences for the region especially during international consultations. It is useful to learn about specific skills needed to create an authentic video visit also referred to as ‘webside manners’. These include ensuring that appropriate ‘eye contact’ is created mimicking in-person interaction, avoiding talking over the other person or waiting too long to respond, providing timely cues about turn taking, using facial expressions to relay natural emotions like empathy, concern, surprise etc. In addition, it is important the individual on the other end feels heard, comforted and validated during the virtual interaction.

Pic 2. Using non-verbal cues during telepsychiatry visit (Copyright: David Roth, MD with permission)
Although the principles of clinical care are identical irrespective of it being an in-person or telehealth visit, there are unique considerations for telepsychiatry due to technology and regulations that may vary across different countries. It is imperative to check with the state or national regulations about licensing requirements, reimbursement rules, compliance needs and privacy considerations when reaching non-clinical settings like schools, homes and juvenile prisons before setting up the program. When it comes to technology requirements, a good quality camera, microphone and screen, and the reasonable bandwidth of internet connection are needed. The standard laptop or desktops could be adequate to conduct an acceptable telehealth visit specially in psychiatry because the need for physical exam that needs peripheral tools is minimal. Due consideration is needed for appropriate lighting and minimizing distractions (visual and voice) in the surrounding during videoconferencing.

Pic 3. Conducting telepsychiatry visit on an office computer (Copyright: David Roth, MD with permission)
By increasing access, telepsychiatry holds promise to reduce disparities and improve health outcomes for youth in underserved communities and nations with limited workforce of trained child and adolescent mental health providers. It also has a potential to enhance physician satisfaction, reduce feelings of isolation and access specialty consults without the need for travel, so that they can do their best for wellbeing of their communities.
There are several resources available on the topic and the relevant topics for child and adolescent psychiatrists are included in the ‘Telepsychiatry toolkit’ compiled by the American Academy of Child and Adolescent Psychiatry (AACAP). In addition, the guidelines, best practices and tools for delivery of care using telepsychiatry are also available. The toolkit and other resources can be freely accessed at https://www.aacap.org/AACAP/Clinical_Practice_Center/Business_of_Practice/Telepsychiatry/Telepsych_Home.aspx.